Synopsis
The American Physical Therapy Association (APTA) and its regional chapters have successfully advanced the cause of direct access for physical therapists, positioning them as primary care specialists for musculoskeletal health. This achievement has led to the expansion of direct access permissions across states, with therapy providers becoming initial points of contact for patients seeking musculoskeletal injury care. A notable accomplishment of APTA is the revision of imaging restrictions for physical therapists, allowing them to recommend X-rays and MRIs. While therapists in military settings long enjoyed this privilege, extending it to civilian contexts required persistent efforts. Despite progress, the article highlights the challenge of overused diagnostic procedures like MRIs and X-rays in primary care practices, contributing to healthcare delays and financial strain. The article emphasizes the transformation of physical therapists into thoughtful navigators, leveraging research advancements to provide superior patient care. However, the question remains whether therapy providers should unilaterally decide if further investigation is warranted and if they refer patients for imaging without consulting the referring physician. The answer lies within a close collaboration between therapy providers and physicians, which remains the mainstay of diagnostic referrals. The article emphasizes the added responsibility that therapists now must manage conversations about appropriate investigations with their medical counterparts. It also explores the complex landscape of workers’ compensation, revealing the need for streamlined approval processes. While direct access has empowered therapists, the onus is on them to ensure judicious imaging referrals and uphold their role as industry custodians.
The American Physical Therapy Association and its regional chapters have effectively advocated for a range of privileges linked to direct access, elevating physical therapists’ standing to that of preferred primary care specialists for musculoskeletal health. As a result of these efforts, a majority of states have now extended direct access permissions to physical therapists, and an increasing number of healthcare networks are turning to therapy providers as the initial touchpoint for patients seeking care for musculoskeletal injuries. This emerging pattern is most prominent in outpatient settings, yet it is also progressively gaining traction within acute care environments. A noteworthy accomplishment attributed to the APTA is the revision of imaging limitations for physical therapists across various states. While physical therapists in military settings have benefited from this privilege, achieving the same for therapists in civilian contexts has been a hard-won battle.
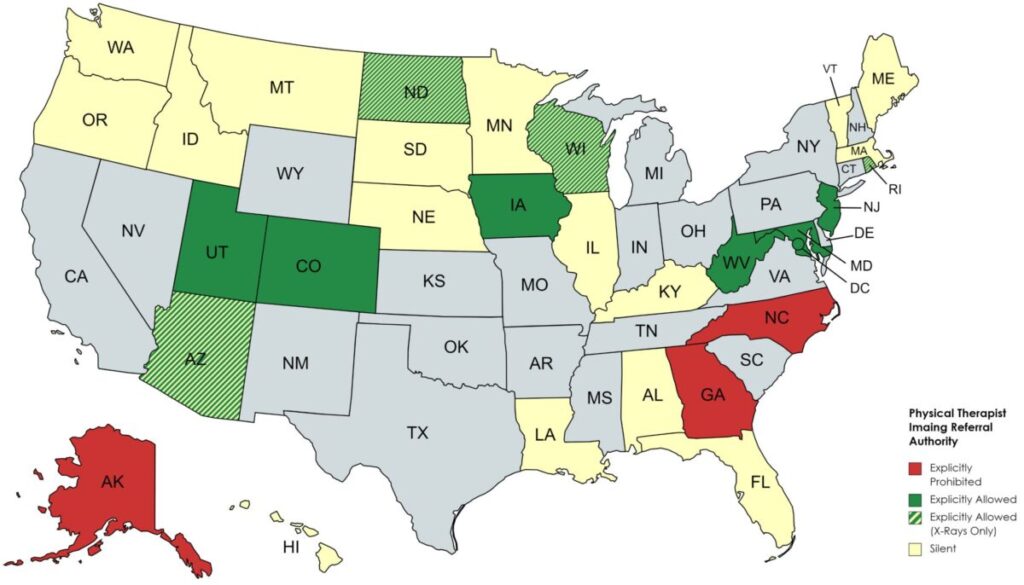
Physical Therapy Imaging Referral Authority Per State
(Source: Lance Mabry, PT, DPT, OCS, FAAOMPT, Redefine Health Education)
Through persistent determination and painstaking effort, this endeavor has gradually gathered momentum, resulting in the inclusion of numerous states on the roster of those where therapists are authorized to recommend X-rays and MRIs for patients. A recent example is Iowa, where therapists have gained the authority to request MRIs and X-rays, while physical therapists in Rhode Island are now empowered to order X-rays.
The Surge of MRI & Diagnostics Overuse and Its Impact on Healthcare Cost & Access
Research has identified excessive utilization of MRI and other diagnostic procedures as a primary contributor to delays in administration and the escalating financial burden within consumer health, Medicare, and workers’ compensation services. Numerous experts have extensively investigated the consequences of unnecessary referrals for diagnostic tests and their associated strain on the American healthcare system. In a five-year retrospective analysis, Keil et al. (2019) revealed that primary care physicians directed as many as 25% of patients toward X-rays and 11% toward MRIs, figures significantly higher than their counterparts in therapy. Another study identified an inappropriateness of up to 26% of diagnostic imaging referrals made by primary care physicians (Lehnert & Bree, 2010). This pattern has been substantiated by various other research endeavors, prompting the inclusion of MRI and X-ray overuse as a component of 5 areas of physicians’ responsibilities in containing healthcare expenses. This augmented financial load has sparked concerns, particularly in relation to the incorporation of X-ray and MRI referrals within the scope of direct access provision by physical therapists. As a result, this issue has ignited debates within the healthcare community.
Evidence of Physical Therapists as Thoughtful Navigators & Decision-Makers of Diagnostic Referrals
The realm of physical therapy has undergone notable positive transformations and attained an elevated position in recent decades. This evolution is evidenced by the increased adoption of physical therapists as the preferred choice for addressing musculoskeletal injuries. This shift can be attributed to an augmentation in the volume and quality of research and its application, resulting in advancements in PT education, treatment methodologies, and the refinement of skills essential for differential diagnoses. Due to these advancements, the recognition of PT as a reimbursable healthcare service has expanded across a broader spectrum of insurance networks. Moreover, consumers increasingly accept self-payment options related to therapy and wellness services. The advantages stemming from these improvements are evident through early patient exposure to therapy interventions and closer collaboration between therapy providers, physicians, and specialists. These collaborative efforts have further facilitated therapists in acquiring the necessary skills for ordering diagnostic imaging. Substantiating these advantages, studies examining the appropriateness and efficacy of diagnostic referrals by therapy providers indicate that physical therapists exercise greater caution when directing patients toward diagnostic assessments and surgical consultations compared to physician groups. A study by Rabey et al. (2009) showcased that 79% of patients’ complete care episodes were overseen by physical therapists, with merely 9% referred for surgical consultations, 13% for X-rays, and 10% for MRIs. Notably, 89% of those referred for surgical opinions were deemed appropriate referrals. Additionally, Keil et al. (2019) demonstrated that physical therapists exhibited a remarkable level of appropriateness (91%) in their referrals, while the overall number of imaging referrals remained low (9% for X-rays and 4% for MRIs).
Workers’ Compensations: Navigating Challenges & Approval Processes
Workers’ compensation encounters notable complexities in delivering patient care. While the objective of worker’s compensation healthcare is to expedite the reintegration of injured workers into their jobs and provide rightful Compensation, the entire process is riddled with protracted procedures and delays. These challenges largely stem from inadequacies in establishing streamlined approval mechanisms for a range of services, encompassing diagnostics, medical treatments, therapeutic interventions, and surgical procedures. The sequence commences when the injured employee notifies their employer about the injury, prompting the initiation of a claim that is subsequently forwarded to the insurance provider. Upon receiving the claim application, the payers conduct a comprehensive evaluation of the injury claim and, if deemed appropriate, trigger the commencement of initial medical appointments. The specific nature of these appointments is contingent upon whether the state operates under panel or non-panel arrangements. During these appointments, physicians conduct assessments and prescribe essential diagnostics, medical interventions, therapies, and surgical procedures as necessary through written or electronic prescriptions. Given the stringent prerequisites of worker’s compensation, any additions or modifications to the recommended services must be meticulously documented and substantiated by all involved stakeholders, with the medical provider assuming the pivotal role of being the central coordinator for the patient’s care.
Optimizing MRI Referral & and Utilization in Workers’ Compensation Care with Therapist-Physician Collaboration
Similar to consumer health, physicians’ excessive use of diagnostic procedures, particularly MRI scans, remains a persistent concern in work-related injuries. Numerous authors, including Clendenin et al. (2016), have highlighted this issue. The authors have underscored that the annual cost associated with MRI usage has surged to approximately $100 billion, which stands in direct contradiction to the guidelines established by the American College of Radiology, American College of Occupational Medicine, and Official Disability Guidelines. In the preceding sections, we have discussed how the introduction of direct access has empowered therapists to become the preferred caregivers for musculoskeletal injuries, leading to decreased treatment durations, superior clinical outcomes, reduced injury-related costs, and decreased disability claims within the realm of workers’ compensation. However, we must acknowledge the additional responsibility placed upon therapy providers to avoid contributing to the burgeoning healthcare cost burden through unnecessary MRI and X-ray scan referrals. With early access to rehabilitation, patients now have the advantage of prompt physical therapy intervention, which accelerates tissue healing potential.
Consequently, best practices dictate a heightened collaboration between therapy providers, primary care physicians, and specialists. This collaboration streamlines care coordination, improves clinical justification, and reduces administrative and clinical delays that patients might otherwise encounter during transitions between providers or specialties—such as primary care, diagnostics, orthopedic, and pain management care. Coordinated efforts between therapists and physicians have become integral to delivering exemplary patient care, significantly impacting cost containment associated with avoidable specialty referrals and diagnostic overuse. The onus now rests on therapists, who are at the forefront of patient care, to initiate discussions with medical providers about the timing and necessity of appropriate investigations. This is particularly relevant when a patient’s progress has plateaued or declined. However, an ongoing debate continues around determining the best approach for referring patients to diagnostic imaging:
Should therapy providers independently decide if further investigation is required, or is it more appropriate to collaborate with the referring physician before making such recommendations?
The issue, as we recognize, is not about a therapist’s competency in identifying the need for imaging for an injured worker. What is problematic is the common practice among therapy providers to suggest the necessity of an MRI or surgery directly to the patient, bypassing communication with the primary care physician or specialist. This practice not only generates anxiety and trepidation about further medical evaluations but also needlessly entangles patient care in legal matters, which is entirely preventable and detrimentally impacts patient care and experience. This primarily happens due to the following areas of concern:
- Blame. Blame represents a psychological response to manage a harmful incident, often with profound implications for one’s life. In the context of workers’ compensation, this pertains to injuries sustained at work. When an employee is injured, they tend to form judgments and search for someone to take responsibility for the injury, pain, delayed or incomplete recovery, and challenges in returning to work. Simultaneously, they try to understand the cause and facilitate their recovery independently or in collaboration with their families and lawyers. Rosenthal & Schlesinger (2002) argue that in most severe cases, the patients are willing to play the conventional “sick role” and grant complete authority to their providers, thereby making these providers less subject to blame. Unfortunately, inadequate communication between therapists and physicians and misinformation gathered by the injured employee about the necessity of medical imaging exacerbate the situation. This leads patients to question their doctors’ and employers’ intentions, harboring suspicions against them. The situation worsens when physicians fail or are not inclined to provide a convincing rationale for postponing or denying imaging referrals, neglecting patients’ pre-existing biases.
- Payor-Receiver Bias. According to the principles of pricing psychology, the amount a customer spends indicates the perceived worth and caliber of a product or service. When a service is rendered at a minimal expense or without charge, customers are left uncertain about its true value. Within the realm of Workers’ Compensation, discontentment with the care strategy already exists due to the disparity between those procuring the service (employers) and those benefiting from it (injured employees), where the procurer is not directly covering the service costs. Consequently, any compromise in the genuine or perceived quality or intention of the care further exacerbates an unfavorable reaction, which in this case arises due to inconsistent or misinformation rendered by the therapy providers regarding the need for imaging, which may be in contrast to a recommendation already made by the medical provider. This dilemma within the employee and the physician relationship intensifies the patient’s tendency to attribute blame, often directed at medical providers and, in most instances, at the payer and the employer.
- WC Value Chain and the Role of Workers’ Compensation Physicians. The role of a designated healthcare provider involved in workers’ compensation, whether they are a primary care physician, an occupational health specialist, a trauma expert, a physiatrist, or an orthopedic specialist, is pivotal within the worker’s compensation framework. They serve as central coordinators, responsible for the initial medical diagnoses (which is a pre-requisite for receiving workers’ compensation benefits), referring injured workers to subsequent diagnostic, medical, surgical, and therapeutic interventions, issuing job restrictions and/or modifications, and assessing the level of impairment and disability. Additionally, they create documentation that serves as evidence for medical and legal justifications. In workers’ compensation, physicians serve as the nexus for all communications and approval processes. Therefore, it stands to reason that maintaining an open line of communication between therapy providers and medical professionals—verbal or written, such as emails or clinical documents—is in the best interest of patients, especially when it pertains to requested services like imaging.
Conclusion
Implementing direct access to physical therapy has fundamentally reshaped the role of therapy providers within musculoskeletal care. They have assumed the central role as the initial point of contact for patients throughout their healthcare journey, extending their influence on the workers’ compensation industry and guiding employees from prevention to returning to work. Furthermore, by being able to recommend imaging, therapists have broadened their responsibilities in steering injured workers toward optimal health results. Nevertheless, past trends in the industry have underscored the necessity for caution to prevent unwarranted MRI referrals, which can result in excessive administrative and financial strain.
To mitigate this risk, it is imperative for medical and therapy providers to collaborate closely to determine the appropriateness of imaging. Additionally, it is advisable to exercise discretion when discussing the need for imaging with injured employees, instead relying on referring medical providers to guide patients toward imaging and surgical recommendations. This approach is crucial for advancing patient care while mitigating potential legal and medical complications. Therapists now bear the responsibility of initiating these conversations and maintaining their role as exemplary stewards of the industry they proudly represent. In conclusion, through collaborative efforts and careful oversight, healthcare providers can ensure optimal patient outcomes while minimizing unnecessary burdens.

